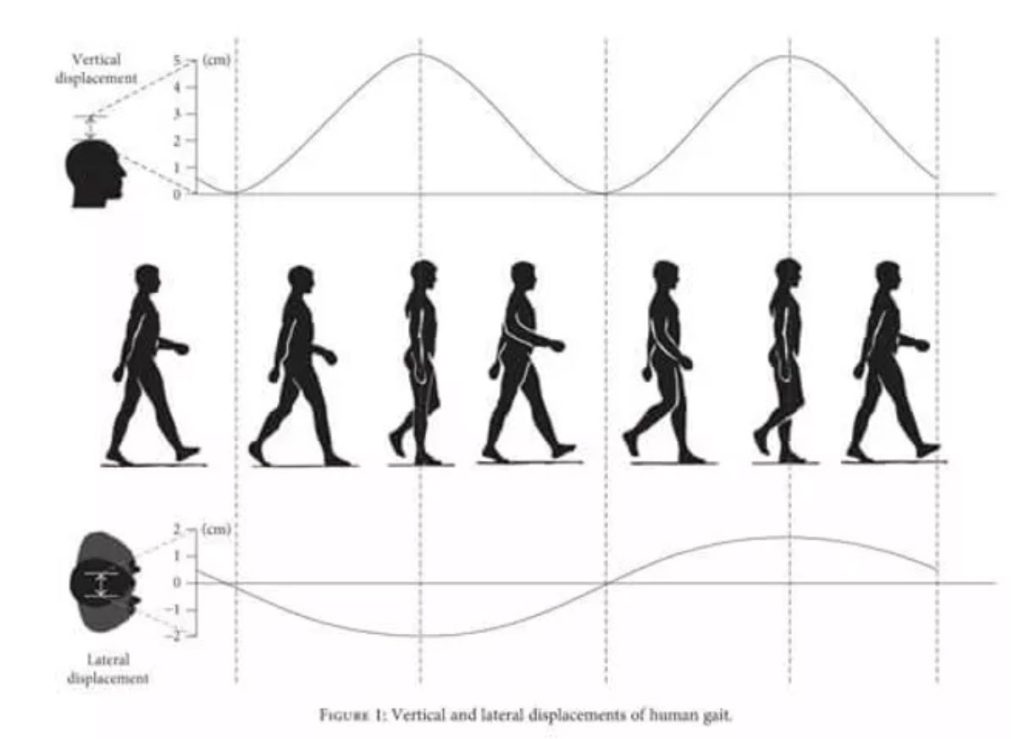
The Vestibulo-Ocular Reflex (VOR) is a reflex that produces compensatory eye movements in response to head movement. The eye movements are equal in amplitude and speed to the head movement, but in the opposite direction. The goal of this reflex is to ensure stable gaze during head movements to minimize blurring of visual targets perceived in the environment. Those with reduced VOR function (i.e. vestibular disorder) cannot produce sufficient compensatory eye movements to compensate for their head movements. As a result, a common complaint is visual blurring during motion – this is called oscillopsia (check out video below – caution: can be symptom provoking!). As our head and body are constantly moving, a clear image during movements is important. Even when we are walking straight and looking ahead, our heads naturally bob up and down and move side to side (refer to image below). Imagine if we couldn’t keep our vision stable as we moved around, it would be dizzy and nauseating – no wonder those symptoms are common after a concussion or vestibular disorder!
BEWARE: Watching this video can be symptom provoking!
Vertical and horizontal head displacement during gait
VOR TESTING
VOR Testing is one component of a comprehensive Vestibular Assessment, and some physical assessments that specifically evaluate for VOR function include:
HEAD IMPULSE TEST (OR HEAD THRUST TEST):
The Head Impulse Test is a common bedside test involving turning the patient’s head abruptly to observe for whether they are able to maintain a steady gaze on a target during the movement. An abnormal result is indicated when the patient is unable to maintain a steady gaze on the target and can show whether the patient has a unilateral or bilateral loss of VOR function.
DYNAMIC VISUAL ACUITY TEST:
The Dynamic Visual Acuity Test is a bedside test that involves passively turning the patient’s head at a certain speed while having them read lines on an eye chart. An abnormal result is indicated when the patient’s ability to read the lines on an eye chart is significantly different during head movements compared to when their head is still.
HEAD SHAKING NYSTAGMUS TEST (WITH INFRARED VIDEO GOGGLES):
The Head Shaking Nystagmus Test is a test that involves oscillating the patient’s head for a certain number of repetitions, followed by observing the eyes for nystagmus (a type of eye movement). It is typically performed with infrared video goggles in order to have a clear view of the eyes. As the eye movements can be very subtle and imperceptible, it is important to be assessed by a properly trained vestibular therapist who has had the training to observe for these eye movements.
As the vestibular system can detect and appropriately respond to a broad range of head velocities, it is important to train across a variety of speeds. Walking and most activities of daily living may predominantly use lower head velocities and running requires a higher head velocity, so training across a broad range of head velocities is beneficial for a full return to daily activities. The goal of improving VOR function is to normalize gaze stability and postural control, by reprogramming eye movements and postural responses to movement.
___________________________________________________________________________________________
As a Vestibular Therapist, when I prescribe exercises to improve VOR function, I consider whether the patient’s symptoms are provoked by specific movements, positions, or environmental situations, as treatment is guided by the specific symptoms reported by the patient. The diagnosis has less relevance in my considerations in creating a plan for their Vestibular Rehabilitation program. What is more important is that the exercises are closely supervised and progressed appropriately, as it is easy to either overdo them, such that the symptoms are significantly aggravated, or “underperform” them in such a way that the exercises are not effective.